What is Astigmatism?
Astigmatism is a common refractive error of the eye, akin to myopia (near-sightedness) or hyperopia (longsightedness).
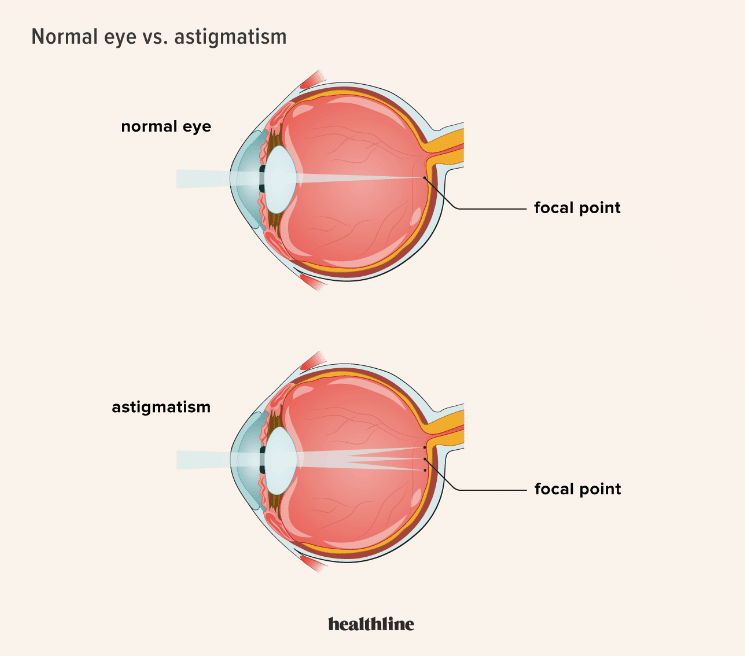
Astigmatism occurs when the cornea or lens of the eye has an irregular shape, causing light to focus unevenly on the retina. It can exist alongside myopia or hyperopia, or on its own.
What Causes Astigmatism?
There are two meridians, usually at right angles to each other.
In astigmatism, these meridians have different curvatures, one being steeper and the other being flatter. This uneven curvature causes light to focus on multiple points rather than a single point on the retina, resulting in blurred vision.
Factors that put an individual at a higher risk of developing astigmatism:
- Genetics, where one or both parents have astigmatism
- A corneal scar after an ocular surgery or injury
- Keratoconus, a rare eye condition where the cornea progressively thins and bulges
- Congenital abnormalities or degenerative disorders
Illustration of normal vs. astigmatic corneas
Recognizing the Symptoms of Astigmatism
Due to light rays focusing at different points on the retina in individuals with astigmatism, it will cause images to appear blurred or ‘fuzzy’.
Individuals may also experience other symptoms like eye strain, and headaches due to squinting. It increases difficulty seeing at night or in low-light conditions.
Real-life examples of blurred vision scenarios
- Driving in low-light conditions makes seeing road signs, traffic signals, and other vehicles difficult.
- Fine detail tasks such as reading small print, threading needles, or working on intricate crafts can be challenging.
Diagnosis of Astigmatism
Diagnosing astigmatism involves a comprehensive eye examination conducted by an optometrist or ophthalmologist.
- The patient’s visual acuity (VA) will be assessed, where the eyecare practitioner identifies visual impairments if any.
- Measurement of the refractive error of the eye through the refraction test. The practitioner uses corrective lenses to assess the power of myopia, hyperopia, and/or astigmatism.
- After the patient’s refractive error has been determined, they will be given a prescription. It would typically be written in the format shown below:
-
SPHERE CYLINDER AXIS VISUAL ACUITY Right Eye -3.00 -0.75 180 6/6
-
“SPHERE” is the refractive power indicating if the patient is myopic (minus power) or hyperopic (plus power). An individual can only either be myopic, or hyperopic.
“CYLINDER” is the refractive power of astigmatism in the patient, and this is typically corrected by a cylindrical lens.
“AXIS” is the meridian where the steepest curvature of the cornea is.
Corneal topography is a diagnostic imaging technique that is used by practitioners when astigmatism is suspected.
Treatment Options for Astigmatism
#1 Eyeglasses
The most common and simplest treatment for astigmatism. Toric lenses can be customized to correct both spherical and cylindrical components of an individual’s refractive error.
Pros
- With the ability to customize the lenses to an individual’s refractive power, eyeglasses can provide precise and consistent correction for astigmatism.
- Convenient as they can be quickly worn and removed as and when needed.
- Frames comes in a variety of materials, and designs which individuals can choose to suit their personal preferences.
- Physical protection for eyes against environmental hazards like dust, debris, and harmful UV rays.
- Often more affordable with minimal expenses required for maintenance.
Cons
- Increased peripheral distortion in individuals with a higher prescription.
- Individuals may experience the “swimming” effect and find it difficult to adapt to new frames or new refractive powers.
- Inconvenient and impractical for activities where they can be easily displaced or damaged.
- Tend to fog up in cold or hot conditions.
#2 Contact lenses
Toric soft contact lenses (SCL) and rigid gas permeable (RGP) lenses are available in designs that provide clear vision for individuals with irregular corneal shapes. Those with higher power of astigmatism would benefit from a different RGP-material lens known as the “scleral lens.” It provides vision correction and comfort.
Pros
- Provides a clear and natural field of vision.
- Provides an aesthetic advantage for many individuals.
- With the freedom of movement, there are fewer opportunities to displace or damage one’s visual aid.
Cons
- Adaptation period for first-time contact lens users where they may experience discomfort or irritation during wear.
- Increased risks of developing eye infections may arise from improper contact lens care regimens or lack of hygiene practices while handling contact lenses.
- Regular contact lens reviews are required to ensure the contact lenses are well-fitted.
- A high commitment to lens care is required – cleaning, disinfecting, and replacing lenses on a regular schedule.
- Contact lenses and cleaning solutions can be costly.
- Some individuals may have certain pre-existing contraindications, or lifestyle factors that make contact lens wear unsuitable.
#3 Refractive surgery
Refractive surgery offers a permanent solution for correcting refractive errors by reshaping the cornea to improve its curvature and focusing ability. When considering this option, a detailed assessment is required to assess the patient’s suitability.
Types of refractive surgeries:
- Laser-Assisted In Situ Keratomileusis (LASIK) – A thin flap is created on the cornea and a laser is used to reshape the underlying cornea tissue. The flap is then repositioned, and the cornea heals naturally.
- Photorefractive Keratectomy (PRK) – Reshapes the cornea’s surface by removing the epithelial, the outer layer, before the laser treatment, instead of creating a flap like LASIK.
- Small Incision Lenticule Extraction (SMILE) – Creates a small incision in the cornea to remove a small piece of tissue, known as lenticule, to reshape the cornea to correct for refractive error.
- Implantable Collamer Lenses (ICL) – Permanent contact lenses placed inside the eye to correct for refractive error. The procedure is reversible and corrects a wide range of prescriptions.
Lifestyle Tips for Managing Astigmatism
- Ensure glasses are correctly prescribed.
- Ensure proper lighting when reading or performing close-up tasks to minimizes eyestrain.
- Avoid rubbing the eyes
FAQs
- Question: Can astigmatism be inherited?
- Answer: Yes. Astigmatism has a genetic component and can run in families.
- Question: How often should I get my eyes checked for astigmatism?
- Answer: An eye check once every two years is sufficient if an individual is well.
- Question: Are there natural remedies to improve astigmatism?
- Answer: There are no scientifically proven natural remedies to cure or reverse astigmatism.
- Question: Can astigmatism get worse over time?
- Answer: Yes, astigmatism can worsen over time for some individuals.
- Question: What are the risks associated with refractive surgery for astigmatism?
- Answer:
- Undercorrection or Overcorrection. Undercorrection may require enhancement procedures to improve vision, while overcorrection may necessitate corrective lenses or additional surgical interventions.
- Induced Astigmatism after surgery
- Glare, Halos, and Starburst
- Corneal Ectasia
- Answer:
- Question: Is astigmatism only corrected with glasses or contacts?
- Answer: No, astigmatism can be corrected through refractive surgery as well.
- Question: Can children develop astigmatism?
- Answer: Yes, children can develop astigmatism. Astigmatism can occur at any age, including infancy and childhood.
- Question: Are there specific foods that can improve astigmatism?
- Answer: There is no direct evidence to suggest that specific foods can improve astigmatism.

